What is childhood cancer?
“Cancer” refers to a group of illnesses. Every type of cancer has its own name, characteristics, treatment and chances for curing. Cancer means that certain cells in the body lose control over their growth. These cancer cells multiply inappropriately and live longer than normal cells. A group of cancer cells is called a “tumour”. Sometimes cells can be released from the tumour and can circulate through the blood to other parts of the body, where they can form new tumours, called metastases.
Paediatric cancer is relatively rare: it makes up less than 1% of all cancer cases. In Belgium, this means that approximately 320 children younger than 15, and 180 adolescents between 15 and 19 years are diagnosed with a certain type of cancer each year. This means that approximately one in 300 young adults has had cancer as a child.

Cancer in children and adolescents by tumour type
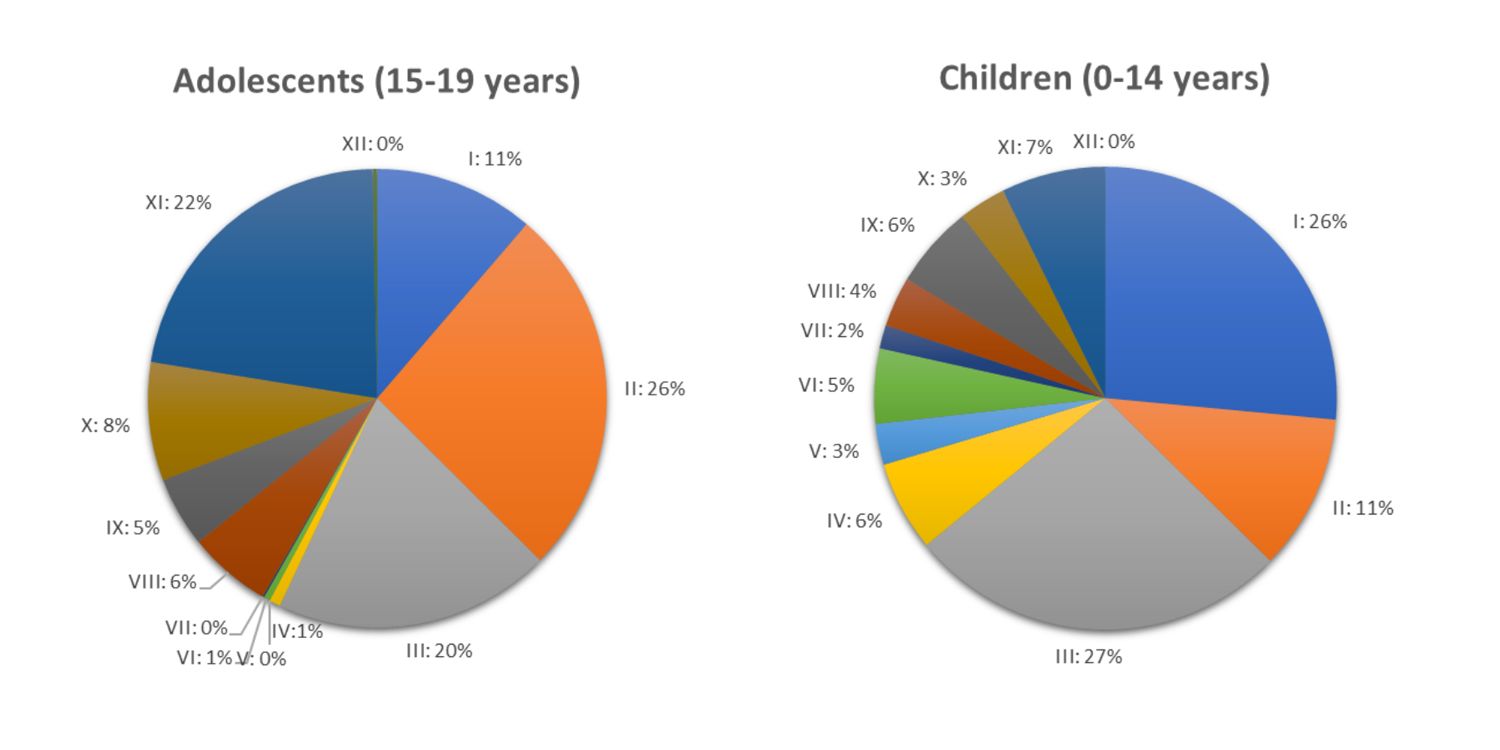
Legend
- Leukaemia
- Lymphoma
- CNS
- Neuroblastoma
- Retinoblastoma
- Renal tumour
- Hepatic tumour
- Malignant bone tumour
- Soft tissue sarcoma
- Germ cell tumour
- Other neoplasms and melanomas
- Other
Cancer occurs less frequently in children than in adults and cannot be compared to adult cancer. While In adults, the most common types of cancers are cancers of the skin, breast, prostate, lung and colon; the most common types of cancers in children are those of the blood and bone marrow, lymph nodes, brain, muscles, kidneys and bone. In general, children respond better to treatment compared to adults.
When searching the internet for information regarding paediatric cancer, please always keep in mind that this information may not be reliable or accurate. Parents are strongly advised to discuss the information they found with their doctor, who knows their child’s specific details.
What are the diagnostic procedures?
To determine whether cancer is present in the body and which type of cancer, the child will need to have several procedures, depending on the signs or symptoms. The following procedures are possible:
Biopsy
With a biopsy, a small piece of the tumour can be investigated in the laboratory for diagnosis. There are 2 types of biopsy:
The biopsy is sent to a laboratory to be examined by a pathologist. He investigates whether the cells in the biopsy are cancerous and which type of cancer it is. It takes several days before you get the results.
- A needle biopsy: a needle is put into the tumour through the skin to remove a small piece of the tumour. This biopsy can be done under local or general anesthesia.
- An open biopsy: during a minor surgical intervention under general anesthesia, a piece of the tumour is taken out. The surgeon may sometimes be able to remove the entire tumour.
Bone marrow puncture
The bone marrow is a liquid spongy tissue inside the bones that produces the different types of blood cells. A bone marrow puncture is performed to examine whether the cells in the bone marrow are healthy and present in sufficient quantity. During the procedure, a needle is placed in the bone (usually the hip bone) and a small quantity of bone marrow is drawn out with a syringe. This bone marrow sample goes to the laboratory for analysis. This procedure is usually done under general anesthesia and is combined with other examinations when possible. The bone where the sample is taken from might feel sore for a few days.
Bone marrow biopsy
A bone marrow biopsy is performed to examine the blood cell precursors in their natural environment, so in the bone itself. During this procedure, a needle is placed in the bone (mostly the hip bone) and a small piece of the bone is removed. This procedure is usually combined with a bone marrow puncture and the same skin puncture place is used for both procedures. The bone marrow biopsy piece is examined in the laboratory. This procedure is usually done under general anesthesia and is combined with other examinations when possible.
Lumbar puncture
A lumbar puncture (or LP) is performed to investigate whether any cancer cells are present in the fluid around the brain and the spinal cord. A hollow needle is placed between the vertebrae (spinal bones), where the fluid is located. The fluid then drops from the needle into a test tube which is sent to the laboratory for analysis.
For some types of cancer, treatment with chemotherapy is injected via the needle after the fluid has been taken. After this procedure the child has to lie down for a while to make sure the medication spreads equally in the fluid around the spinal cord. This procedure is performed under a general anesthesia or proper premedication.
X-rays
An x-ray is a photo that shows the inside of a body. A tumour often looks different from healthy tissue when seen on an x-ray. The photo can show if there’s a mass in the chest, abdomen or bones. An x-ray doesn’t take long and is not painful.
Ultrasound
An ultrasound is another imaging technique that doesn’t use x-rays. The ultrasound machine uses sound waves to create images. The operator or radiologist will apply a cold gel on the body and will place a probe on the area to be examined. It is the same technique that is used to examine unborn babies in pregnant women.
CT scan and MRI scan
A CT scan is a special kind of x-ray that shows more details than ordinary x-rays. Sometimes a contrast fluid is injected to improve the contrast between different anatomical structures on the images.
An MRI scan is similar to a CT scan, but it uses magnetism to obtain a detailed picture instead of x-rays. This means that there is no radiation involved. The patient cannot take any metal items with him/her, because of the magnet in the machine. For an MRI scan, you have to lie down in a very noisy machine for 20 minutes or longer. For young children, an MRI may be performed under general anesthesia to allow for immobilization during the exam.
PET-CT-scan
In some cases of solid tumours or lymphoma, the presence or absence of metastases can be assessed by performing a PET-CT scan. A small dose of radioactive substance (sugar) is injected into a vein which will localize the areas of the body where metabolism is active and the sugar is utilized. This is combined with a CT scan to better assess the anatomical regions where the metabolism is increased. For this examination, it is important to have fasted for at least 6 hours to avoid any possible interference between the injected sugar and the sugar already in the blood. It is also important to keep warm in order to avoid an increased uptake of the tracer in brown fat. For young children, this exam may be performed under general anesthesia to allow for immobilization during the scan.
Bone scan
If your child has a bone tumour or a tumour that may have spread to the bones, a bone scan will show how much bone is affected. During the bone scan, a small dose of a radioactive substance (tracer) is injected into a vein that can be absorbed by the bone. Abnormal areas of bone will absorb more of the substance and will highlight on the scan. The radiation dose is very low and not harmful.
MIBG
MIBG-(meta-iodobenzylguanidine) is a substance that is present in some tumours, particularly neuroblastoma. Before the MIBG scan, a small amount of radioactive iodine (tracer) is injected intravenously and will be absorbed by the tumour cells. Pictures are then taken under a scanner that is similar to a CT scan. On the images, bright spots will be visible where the tumour cells are located. MIBG scans are helpful for locating both bone and soft tissue tumours. A special medicine (lugol) is given to protect the thyroid gland from the radioactive substance in the tracer. For young children, this exam may be performed under general anesthesia to allow for immobilization during the scan.
Blood analysis
The different types of blood cells are counted (red blood cells, white blood cells and platelets) and blood can be analyzed to assess kidney and liver function and if there are signs of infection. Not every test is done every time. In some types of cancer, tumour markers can be traced in the blood.
Urine analysis
A urine analysis can help to assess the kidney function and whether the urine is infected. In some types of cancer, a tumour marker can be traced in the urine.
Audiogram
Some cancer treatments can affect the child’s hearing. To assess hearing function before, during and after treatment, an audiogram is performed. The test takes place in a quiet room and the child will be asked to listen to sounds at different frequencies through headphones.
Echocardiography
Some cancer treatments can affect the function of the heart. An echocardiogram is an ultrasound of the heart and shows how strong it is and how well it works. A gel is spread on the chest and a probe producing sound waves is passed over the chest. The sound waves are converted into an image.
Electrocardiogram (ECG)
An ECG measures the actvity of the heart. Small electrodes are placed on the chest, arms and legs and attached to a machine which will produce a trace.
Cr-EDTA scan (or test or scintigraphy)
A Cr-EDTA scan is another test to assess the kidney function. A small amount of radioactive tracer (Chrome-EDTA) is injected in a peripheral vein. At specific time points a blood sample is taken to measure how quickly the tracer is eliminated from the body. A Port-a-cath or any other venous access device cannot be used for this test as it leads to tracer accumulation and erroneous interpretation of the results.
What are the types of childhood cancer?
To determine whether cancer is present in the body and which type of cancer, the child will need to have several procedures, depending on the signs or symptoms. The following procedures are possible:
Leukaemia
Leukaemia is a cancer of the white blood cells. White blood cells help to fight an infection. In leukaemia, the production of abnormal white blood cells gets out of control and they continue to divide in the bone marrow without maturing. These immature cells fill up the bone marrow and prevent the production of normal blood cells.
There are two main types of childhood leukaemia:
- Acute lymphoblastic leukaemia (ALL)
- Acute myeloid leukaemia (AML)
Lymphoma
The lymphatic system consist of bone marrow, thymus, spleen and lymph nodes. The lymph nodes are connected by a network of vessels that contain lymph fluid. Lymphoma can start anywhere in the lymphatic system.
There are 2 main types of lymphoma that may occur in children and adolescents, depending on the originating type of cells that become cancerous:
- Non-Hodgkin lymphoma
- Hodgkin lymphoma
Tumours of the central nervous system are, besides leukaemia, the most frequent tumours in children. They can occur in the brain or the spinal cord. There are a lot of different types of brain tumours in children, that vary enormously in natural evolution, treatment options and prognosis. A tumour in the brain can start in the brain itself or can result from the spreading of a tumour from another part of the body (brain metastasis).
The different types of brain tumours are usually named after the types of cells they originate from. The most frequent types are astrocytoma, ependymoma and medulloblastoma. Brain tumours can be benign or malignant. Benign brain tumours are non-cancerous and it is unusual for these cells to spread into other areas of the body. However, they can cause important signs and symptoms when left untreated due to their localization and cause pressure and damage to the surrounding areas in the brain.
- Low grade glioma
- High grade glioma
- Diffuse intrinsic pontine glioma (DIPG)
- Medulloblastoma
- Ependymoma
- Atypical teratoid rhabdoid tumour (ATRT)
- Intracranial germ cell tumour
Osteosarcoma
Osteosarcoma is a malignant type of bone tumour. It is more common in older children and teenagers. Osteosarcoma usually starts to develop at the end of the long bones, which is where new bone tissue is formed when the child grows. The most common sites for osteosarcoma are arms and legs.
Ewing sarcoma
Ewing sarcoma is another type of bone cancer that is usually formed in the long bones, ribs, pelvis and spine. Ewing sarcoma can, in some cases, also occur in the soft tissues.
Rhabdomyosarcoma
Rhabdomyosarcoma is a cancer of the soft tissue, more specifically of the muscle tissue. It can basically develop anywhere in the body, but is most frequently found in the head and neck, bladder, testes, uterus or vagina.
Neuroblastoma
Neuroblastoma is a cancer that develops from primitive cells that are left behind from prenatal development (neuroblasts). Neuroblastoma is the most common cancer in babies and the third-most common cancer in children after leukaemia and brain tumours. Neuroblastoma can develop anywhere in the body, but originates from one of the two adrenal glands or from nerve tissue alongside the spinal cord.
Wilms’ tumour
Wilms’ tumour is the most frequently encountered cancer of the kidney in children. It is thought to develop from immature cells in the embryo (normally these cells disappear at birth).
Germ cell tumours
Germ cell tumours develop from the germ cells, which are the precursor of the reproductive cells (oocyte or sperm). During prenatal development of the foetus, the germ cells producing eggs or sperm normally move to the ovaries or testes. The tumour usually develops in the reproductive system (ovaries or testes) but it can also develop in the brain or another part of the body. Germ cell tumours are sometimes given different names based on what they look like under the microscope. These include yolk-sac tumours, germinomas, embryonal carcinomas, mature teratomas and immature teratomas.
They may be non-cancerous (benign) or cancerous (malignant). Malignant tumours have the ability to grow and spread to other parts of the body.
Immature teratomas fall between benign and malignant tumours. They can occur at many different sites (most commonly in the abdomen)and can spread locally, such as within the abdomen, but rarely beyond. They can usually be surgically removed.
Retinoblastoma
Retinoblastoma is a cancer type of the eye and can occur in the context of a genetic abnormality that predisposes to the development of retinoblastoma (usually young children and bilateral tumours -in both eyes) or sporadically (usually unilateral retinoblastoma – in one eye).
Liver tumours
There are 2 types of malignant liver tumours that occur in children
- Hepatoblastoma: occurs usually in children younger than 5 years old
- Hepatocellular carcinoma: is very rare and occurs in older children or in children with a diseased liver
LCH (Langerhans Cell Histiocytosis) refers to histiocytes, which are cells that are part of the immune system and are found in many parts of the body. There are 2 types of histiocytes:
Langerhans cells are a type of dendritic cells that are normally only found in the skin and airways, but in case of LCH, we can also find them in other parts of the body (bone marrow, liver, spleen,…) where they can cause damage.
- Macrophage/monocyte cells: these cells are responsible for destroying harmful cells such as viruses and bacteria
- Dendritic cells: these cells stimulate the immune system in its defense mechanism
There are 2 types of LCH:
- Single system: only one part of the body is affected
- Multi-system: more than one part of the body is affected
What is the possible treatment?
Every type of cancer has a specific treatment. Which specific treatment will be proposed to a child depends on the current standard of care treatment and the availability of a clinical trial. The doctors will always discuss the current treatment options with the child and his/her family.
Different types of treatment in childhood cancer are possible.
Chemotherapy
Chemotherapy refers to a class of drugs that block cancer cell division and multiplication or that destroy cancer cells. Every type of chemotherapy works in a specific way and the number and combination of drugs that will be prescribed to the child will depend on the type of cancer. When chemotherapy destroys cancer cells, it doesn’t discriminate between cancer cells and normal dividing cells. Therefore the chemotherapy will also destroy normal healthy cells but these normal cells can repair the damage caused by chemotherapy, while cancer cells can’t.
Chemotherapy can be given either as tablets, capsules or liquids that are swallowed, or by injection. Many chemotherapy drugs used in the treatment in cancer, are injected into a vein into the blood stream (intravenous). Intravenous administration of chemotherapy requires the availability of a secure venous access system. There are different possibilities to access the blood stream (Port-a-cath, Hickman or Broviac catheter and PICC-line).
Common adverse effects of chemotherapy are: nausea and vomiting, low blood cell count, mouth ulcers and hair loss. Some adverse events occur immediately upon administration and other may occur at a later time point. The type and the severity of these effects on the long term depend on the type of chemotherapy a child has received. The doctor will always discuss the potential side effects a child may experience, depending on the proposed treatment.
Radiotherapy
Radiotherapy relies on x-rays with a very high energy level that are focused on the tumour to damage or destroy fast growing cells, while doing as little harm as possible to normal cells. When a child receives radiotherapy, the area that is to be irradiated will be measured exactly beforehand. This is called a simulation. Radiotherapy is not painful, but the patient has to lie still during this procedure, so for young children, general anesthesia may be necessary. The doctors and nurses of the radiotherapy unit can give more information about the possible adverse effects of radiation. Radiotherapy will not make a child radioactive and it is safe for them to be with other people.
Surgery
For some cancers, surgical removal of the tumour remains important to treat the cancer. In some cases, this is the only required treatment. However, chemotherapy and/or radiotherapy can be necessary to eliminate any remaining cancer cells and/or to prevent recurrence or metastasis.
Stem cell transplantation
Stem cell transplantation can be useful for high risk leukaemia, as well as for some other cancers or diseases. A stem cell transplant allows a child to tolerate higher doses of chemotherapy. This can improve the survival rate. Before a stem cell transplantation can take place, stem cells need to be collected from the bone marrow or blood. In some cases, the stem cells will be collected from the patient himself (autologous transplantation), in other cases stem cells are collected from a donor (allogeneic transplantation) within the family or from an unrelated donor.
First, the child will receive high doses of chemotherapy and sometimes also radiotherapy to the whole body. The high doses of chemotherapy destroy the remaining cancer cells, but also the stem cells in the bone marrow. After the chemotherapy, the stem cells are infused and these cells will start producing mature blood cells again. When a stem cell transplantation is part of the treatment plan of a child, more detailed information will be given to you by his/her doctor. The child and his/her parents if the child is a minor, will be required to sign an informed consent form, comparable to what is done in the case of a clinical trial.
Immunotherapy
In the last few decades immunotherapy has become an important part to treat some types of cancer. Immunotherapy is a treatment that stimulates the immune system to attack and destroy diseases such as cancer. Immune cells and substances circulate in your body and protect your body from infections and diseases. Once a foreign substance is detected in your body, your immune system attacks and destroys this foreign substance. Cancer cells are often not recognized by your own immune system because cancer cells divide uncontrolled and are often much like normal cells. Researchers were able to develop immune system proteins (antibodies) that specifically recognize a part of the cancer cell (antigen) to block or destroy the cancer cells by your immune system. There are different types of immunotherapy. Depending on the type of cancer, immunotherapy may be a valuable treatment option. Please contact your doctor for more information. While chemotherapy destroys cancer cells and normal cells, immunotherapy binds and destroys cancers cells more specifically. Usually immunotherapy is administered intravenously. The most common side effects of immunotherapy are: chills, fever, rash, low blood pressure, vomiting, diarrhea, headache and weakness.
Targeted Therapy
Targeted therapy is a type of cancer treatment that works by targeting specific molecules or proteins that promote cancer cell growth and spread. Unlike chemotherapy, which can damage both healthy and cancer cells, targeted therapy drugs are designed to attack only cancer cells, without damaging normal cells. Targeted therapy is a group of treatments that work by different mechanisms.
Targeted therapies aim to stop cancer cell growth and division by preventing signals that encourage it, or by activating the immune system to attack cancer cells. They can be given orally or through veins and are usually combined with other cancer treatments, such as chemotherapy, radiation therapy, or immunotherapy.
Targeted therapies have a side effects that are very different in nature from classical side effects of chemotherapy, such as problems with blood clotting and wound healing, blood pressure, hair color changes, skin problems, eye problems etc.























